What is PNE? in Pudendal Decompression Surgery
Revised: 03/20/2020 11:29 a.m.
- March 10, 2020, 1 p.m.
- |
- Public
Pudendal Nerve Entrapment Syndrome
Kaur J, Singh P.
Introduction
Pudendal neuralgia caused by pudendal nerve entrapment (PNE) is a chronic and severely disabling neuropathic pain syndrome.[1] It presents in the pudendal nerve region and affects both males and females. It is mostly underdiagnosed and inappropriately treated, and causes significant impairment of quality of life.
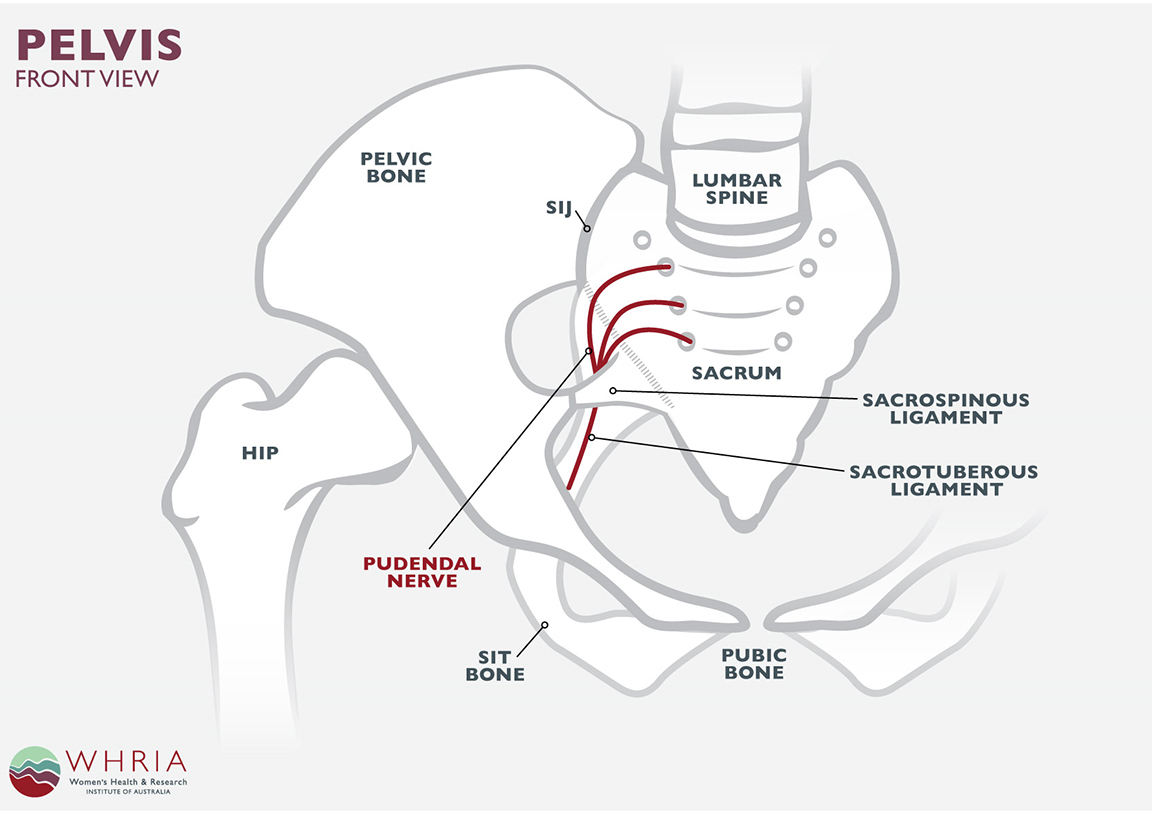
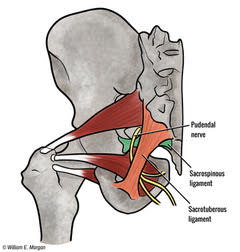
Anatomy of the Pudendal Nerve:
The pudendal nerve emerges from the S2, S3, and S4 roots’ ventral rami of the sacral plexus. It carries sensory, motor, and autonomic fibers, however an injury to the pudendal nerve causes sensory deficits more than motor. It courses between two muscles, piriformis and coccygeus muscles. It departs the pelvic cavity through the greater sciatic foramen ventral to the sacrotuberous ligament. At the ischial spine level, it passes medial to and under the sacrospinous ligament to re-enter the pelvic cavity through a lesser sciatic foramen. The pudendal nerve then courses in the pudendal canal, which is also called the Alcock canal. The three last branches of the pudendal nerve terminate in the ischioanal fossa. These are the inferior rectal branch, perineal branch, and dorsal sensory nerve of the penis or clitoris. However, there are case reports which have shown variability in the anatomy of the pudendal nerve.
Pudendal nerve compression based on anatomy[4][5]:
The pudendal nerve entrapment syndromes subdivide into four types based on the level of compression.
Type I - Entrapment below the piriformis muscle as the pudendal nerve exits greater sciatic notch.
Type II - Entrapment between sacrospinous and sacrotuberous ligaments - this is the most common cause of nerve entrapment.
Type III - Entrapment in the Alcock canal.
Type IV - Entrapment of terminal branches.
Etiology
Pudendal neuralgia can arise from mechanical or non-mechanical injury. The mechanical injury can be due to compression, transaction, or stretching. Amongst the mechanical causes, compression caused by PNE is the most common cause. The non-mechanical causes of pudendal neuropathy include viral infections (herpes zoster, HIV), multiple sclerosis, diabetes mellitus, and others.[6] The first reported case of pudendal neuralgia was due to cycling, which results due to continuous pressure on the Alcock canal.[7]
The causes of pudendal neuralgia are:
1) Pelvic surgery - The surgery for repair of prolapse of pelvic organs is reportedly the most common cause of pudendal neuralgia. The incidence increases if it is a mesh placement surgery; this may require mesh removal in cases of chronic persistent pain.[8][9] It can also develop after mid-urethral sling surgery, hysterectomy, and anterior colporrhaphy.
2) Direct trauma to buttocks or back can also result in pudendal neuralgia.[10]
3) Childbirth - Vaginal delivery causes a significant stretch of pelvic floor muscles by the fetal head, which results in pudendal nerve damage.[11][12]
4) Chronic constipation
5) Excessive cycling - It is presumed to happen because of chronic perineal microtrauma which causes fibrosis in the pudendal canal and also of sacrospinous and sacrotuberous ligaments.[6]
6) Prolonged sitting can also contribute to this condition.
Epidemiology
PNE is a rare syndrome, and the prevalence is unknown. The incidence of this condition as estimated by the International Pudendal neuropathy foundation is 1 per 100,000, but the actual incidence might be higher than reported.[13]
HISTORY
The presenting features of PNE are discussed below[4]
1) It causes pain, numbness, and dysfunction in the distribution of pudendal nerve that includes genitalia, rectum, and terminal urinary tract.
2) Sexual dysfunction, including persistent arousal, dyspareunia, vulvodynia, and male impotence.[14]
3) Sphincter dysfunction presenting as dyschezia, fecal incontinence, and urinary hesitancy.[15]
4) Foreign body sensation in the anus, rectum, urethra, or vagina.
PHYSICAL EXAMINATION
The physical examination in patients with PNE is relatively asymptomatic except for pain reproduction.[16] The symptoms depend on the site of entrapment. If the nerve gets entrapped at the ischial spine or the sacrospinous ligament, it causes pain medial to the ischium. Similarly, tenderness over the greater sciatic notch results when the nerve gets entrapped at, the greater sciatic notch. Entrapment at piriformis leads to spasm and tenderness of piriformis muscle. Lastly, entrapment at the Alcock canal and obturator internus result in tenderness and spasm of obturator internus muscle.
In some of the cases, a transrectal or transvaginal examination might be included in the patient examination to exclude intrapelvic entrapment.
Evaluation
Pudendal nerve entrapment is a potentially challenging condition for physicians to diagnose because there are no specific diagnostic tests. The clinician needs to realize that it is exceedingly mandatory to get a thorough history and perform a detailed physical examination to reach a diagnosis.[17] Dr. Roger Robert published the Nantes criteria to diagnose PNE and appears in detail below. This criterion has validation by many European physicians who have ample experience treating similar conditions.
Nantes criteria:
Inclusion criteria:
1) Pain co-relates with the anatomical distribution of pudendal nerve: Pudendal nerve supplies external genitalia. The pain can be superficial or deep in the vulvovaginal, anorectal, and distal urethra.
2) Pain predominantly in sitting position: This symptom favors nerve compression because if there is a decrease in mobility of the nerve, it makes the nerves vulnerable to compression against hard ligamentous structures. This aspect of pain is dynamic as the pain results from compression and not by sitting position.
3) The patient does not get up with pain at night, although many patients may experience difficulty going to sleep because of pain.
4) There is no sensory loss: The presence of superficial perineal sensory impairment indicates sacral root lesion rather than PNE.
5) Relief of pain with pudendal nerve block: This essential criterion is not specific as any perineal disease other than entrapment can cause pain in the anatomic region of the pudendal nerve. A negative block also doesn’t exclude the diagnosis if there is a lack of precision or when performed too distally.
Complementary diagnostic criteria:
1) Pain is of burning, shooting, or stabbing in nature and associated with numbness.
2) Allodynia or hyperpathia
3) Foreign body sensation or heaviness in rectum or vagina.
4) The pain progressively increases and peaks in the evening and stops when the patient sleeps.
5) Pain is more on one side.
6) Pain more prominent posteriorly and is triggered minutes or hours after defecation.
7) Tenderness felt around the ischial spine during a digital vaginal or rectal examination.
8) An abnormal result on neurophysiological tests
Exclusion criteria:
1) Pain exclusively in the territory not served by the pudendal nerve. It can be in hypogastrium, coccyx, pubis, or gluteus.
2) Pain is associated with pruritus ( more suggestive of a skin lesion).
3) Pain entirely paroxysmal in nature.
4) If imaging abnormality can justify the cause of the pain
Associated signs:
1) Pain in the buttock
2) Referred sciatic pain
3) Pain in the medial thigh (indicates obturator nerve)
4) Pain in the suprapubic region
5) Increased frequency of urine or pain with a full bladder
6) Pain after orgasm
7) Pain worsens hours after sexual intercourse
8) Erectile dysfunction
9) A normal result on electrophysiological tests
Diagnostic tests:
The following tests can help in the diagnosis:
1) Diagnostic blocks: In females, the unguided block can be performed vaginally and in males transperineally. If there is pain relief following the procedure, it indicates that pudendal nerve pathology is the likely cause of pain. The absence of pain relief doesn’t necessarily mean that the patient doesn’t have the condition; it can be because of operative error as well. Image-guided blocks (use of fluoroscopy, ultrasound, CT scan ) increases the efficiency of performance.[18]
2) Quantitative sensory threshold testing works on the principle that compressed nerves cannot detect and transmit changes in vibration and temperature sensation. Thus patients with nerve injury are unable to detect gradual changes in temperature.[19]
High-frequency ultrasonography is helpful in the detection of the site of compression. Compressed nerves appear flat, whereas inflamed nerves appear edematous.[20]
3) Doppler ultrasound has a role in the diagnosis of PNE. As pudendal nerve and vessels course together in a neurovascular bundle, the assumption can be if there is nerve compression, it would also cause vein compression as well, which is diagnosable with a doppler ultrasound.[20]
4) MRI (magnetic resonance imaging) can help in ruling out other causes of chronic pain. The advancement of MRI techniques in evaluating peripheral nerves provides a detailed description of the anatomy, fascicular details, the blood supply of nerve, and 3-D anatomy. [21] It also helps in localizing the site of entrapment.Functional MRI assesses nerve integrity based on their biological properties. Currently, it is considered experimental and inconclusive.[22]
There are no specific and consistent radiological findings in patients with PNE, and further research is necessary for this stream.
If the patient fulfills Nantes criteria, they dont need to undergo any radiological or other investigation to make the diagnosis. However, if the patient lacks any of the criteria, they should be thoroughly evaluated. MRI helps to rule out other causes of chronic pain in such cases.
Treatment / Management
The treatment options are as below:
1) Conservative: Avoidance of painful stimulus is one of the most irreplaceable parts of the treatment. For instance, if cycling causes pain, then either the patient should use proper padding or cease the activity. Similarly, patients who present with pain on prolonged sitting should adopt lifestyle modifications to minimize sitting.
2) Physical therapy: Pelvic floor physical therapy works best for patients in whom pain results from muscle spasms. The physical therapy helps in the relaxation of pelvic floor muscles by releasing spasm and also helps in muscle lengthening.
3) Pharmacologic therapy: The drugs used are analgesics, muscle relaxants, and anticonvulsants (including gabapentin and pregabalin). There are no randomized trials to study and evaluate the efficacy of these drugs.
4) Pudendal nerve block: The other treatment modality is infiltration with local anesthetic or steroid in an area encircling the pudendal nerve. Block can be given unguided or with the aid of ultrasonography, fluoroscopy, or computed tomography (CT) scan. The most consistent technique is with the use of a CT scan.[23]
5) Surgical decompression is considered the best treatment for PNE. The four different approaches are transperineal, transgluteal, transischiorectal, and laparoscopy.[24] All methods destroy nerve fibers. It helps in removing the cause of the compression. Erdogru described a new technique (Istanbul technique) of laparoscopy using the omental flap in 27 patients. The outcome measurement was in terms of pain scores and quality of life. Approximately 81% of patients had more than 80% reduction in pain after six months. Laparoscopy has the advantage of a better surgical field, but it has a learning curve.[24]
6) Neuromodulation: This latest treatment includes the use of peripheral nerve stimulator which causes stimulation of the pudendal nerve in an ischioanal fossa The first case report of this technique by Valovska mentioned the successful management of a patient with pudendal neuralgia with minimally invasive transforaminal sacral neurostimulation.[25]A prospective trial of 27 patients with refractory pudendal neuralgia showed promising results with the use of stimulation of conus medullaris, in which twenty out of 27 patients responded and out of those twenty patients, all had long term relief.[26]
7) Pulsed radiofrequency: Pulsed radio frequency is a relatively new neuromodulation technique and is considered safer than continuous radiofrequency ablation. Current literature suggests that it involves the use of electromagnetic radiation to cause neuromodulation. It is useful for chronic refractory neuropathic pudendal neuralgia.[27]
8) Lipofilling: This is a relatively new technique for the treatment of pudendal neuralgia. Venturi described this technique in fifteen female patients. It requires an autologous injection of adipose tissue along with stem cells in the pudendal canal. The results of ten patients showed decreased pain and a better quality of life at the end of six months.[28] Since this study was of small sample size, and there was no control group, further research in this area is necessary for a more comprehensive application.
Differential Diagnosis
Since there is no confirmatory diagnostic test, pudendal neuralgia is a diagnosis of exclusion. Other conditions merit consideration before making a final diagnosis.[29]
1) Compression by an external source. It can be a tumor or metastasis
2) Superficial infections of the skin in the dermatomes covered by the pudendal nerve
3) Neuropathy of sacral region which is caused by damage to sacral nerve plexus
4) Childbirth: It causes a stretch of the perineum
5) Complex regional pain syndrome, which is a chronic pain condition causes pain in one of the limbs - usually happens after an injury.
Prognosis
Pudendal neuralgia due to PNE affects the quality of life immensely. However, it doesn’t affect life expectancy.
Complications
The complications associated with pudendal nerve block are[30]:
Laceration of the vaginal mucosa
Accidental intravascular injection of local anesthetic can cause cardiovascular and CNS toxicity. The patient can present with palpitation, hypotension, and bradycardia, dysarthria, tinnitus, drowsiness, confusion, loss of consciousness, and convulsions.
Hematoma from injury to the pudendal artery
Infection
Deterrence and Patient Education
Patients should be educated to avoid painful stimulus and actively participate in physiotherapy. Lifestyle modifications are one of the essential elements of the treatment plan.
Pearls and Other Issues
It is very crucial to understand that all types of pudendal neuralgias are not the result of PNE in the treatment planning of patients with chronic pain. It is essential to realize that pudendal nerve can get trapped at different locations, and therefore, all patients cannot receive the same therapy. Patients with chronic pain syndromes tend to get frustrated with multiple failed treatments and can be clinically depressed as well.[31]
A study was conducted by Raynor et al. on 1024 patients to study the prevalence of depression in patients with chronic pain and its impact on health care cost. They categorized 60.8% of patients of chronic pain into probable depression and 33.8% into severe depression based on a questionnaire survey. They also reported higher health care cost amongst patients with depression (p=0.001).[32] Similar results can be seen in data analysis by the medical expenditure panel survey of 26671 patients from 2008 to 2011. The research found that different levels of pain interference increase the total health care cost.[33]
Chronic pain poses a mental and economic burden on the patient. These aspects should be in view when providing holistic care to patients.
Enhancing Healthcare Team Outcomes
Pudendal neuralgia due to PNE is a rare neuropathic condition. It causes a significant impairment of quality of life. It often doesn’t get diagnosed on time, and most patients get treated for other conditions. Thus Nantes diagnostic criteria were established and validated by the an interprofessional team to aid in the diagnosis and further treatment of such patients. If the patient fulfills Nantes criteria, no further investigation is required, however, if any of the criteria are not present, the patient should be further evaluated, and MRI is generally done to rule out other causes of chronic pain. Individualized treatment is necessary. It requires typically permanent lifestyle changes and physical therapy. The treatment options include pharmacological therapy, CT guided blocks, decompression surgery, and neuromodulation.
A well-coordinated interprofessional healthcare team comprised of a pain physician, surgeon, anesthesiologist, nurse, radiologist, and physiotherapist to help in physical rehabilitation, is necessary to treat this challenging neuropathic syndrome. All these disciplines need to collaborate across interprofessional boundaries to optimize care and outcomes. [Level V]
Last updated March 23, 2020



Loading comments...